Peer Reviewed
An Atlas of Lumps and Bumps: Part 14
AFFILIATIONS:
1Department of Pediatrics, University of Calgary, Calgary, Alberta, Canada
2Alberta Children’s Hospital, Calgary, Alberta, Canada
3Toronto Dermatology Centre, Toronto, Ontario, Canada
4Department of Pediatrics and Department of Dermatology and Skin Sciences, University of British Columbia, Vancouver, British Columbia, Canada
5Pediatric Institute, Kuala Lumpur General Hospital, Kuala Lumpur, Malaysia
CITATION:
Leung AKC, Barankin B, Lam JM, Leong KF. An atlas of lumps and bumps, part 14. Consultant. 2022;62(3):e36-e37. doi:10.25270/con.2022.02.00009
DISCLOSURES:
Dr Leung is the series editor. He was not involved with the handling of this paper, which was sent out for independent external peer review.
CORRESPONDENCE:
Alexander K. C. Leung, MD, #200, 233 16th Ave NW, Calgary, AB T2M 0H5, Canada (aleung@ucalgary.ca)
EDITOR’S NOTE:
This article is part of a series describing and differentiating dermatologic lumps and bumps. To access previously published articles in the series, visit https://www.consultant360.com/resource-center/atlas-lumps-and-bumps.
Parulis
Parulis, also known as gum boil, typically presents as an asymptomatic, yellowish or reddish papule or nodule on the gum at the oral end of a draining sinus (Figures 1 and 2). The lesion is usually secondary to a chronic periapical or alveolar abscess, which may result from untreated dental caries.1 The maxillary alveolar mucosa is the most frequent site of a parulis. Causative organisms include Fusobacterium species, followed by Prevotella intermedia/nigrescens, Porphyromonas gingivalis, Tannerella forsythia, and Aggregatibacter actinomycetemcomitans.2,3 A parulis usually perforates spontaneously with purulent discharge into the oral cavity.4 Occasionally, parulides may be complicated by periodontal fistula formation.


Traumatic Fibroma of the Tongue
A traumatic fibroma, also known as irritation fibroma, of the tongue is a benign, exophytic and reactive oral lesion.5,6 The prevalence rate ranges from 1.2 to 77 per 1000 individuals aged 15 to 82 years with a peak in the fourth decade of life.5 The sex ratio is approximately equal.5 The condition results from repetitive tissue injury, which leads to fibrous hyperplasia. The lesion can be tender when rough food comes into contact; this may also occasionally cause the fibroma to bleed.
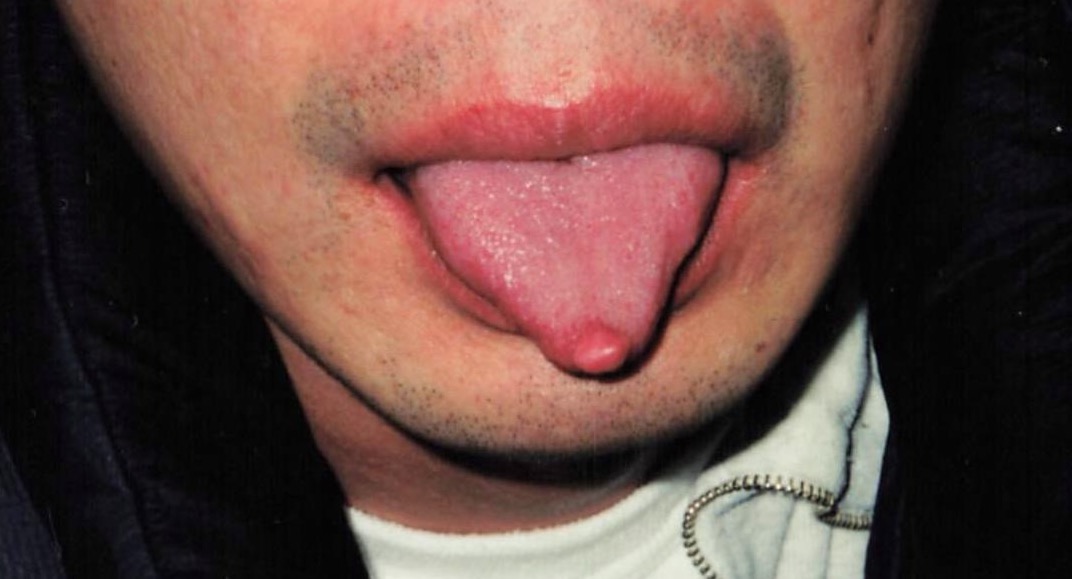
Clinically, a traumatic fibroma of the tongue presents as a sessile, well-circumscribed, firm lesion that is most often located on the lateral aspect of the tongue (Figure 3), followed by the tip of the tongue (Figures 4 and 5). There is no risk of malignant transformation.5


1. Laudenbach JM, Kumar SS. Common dental and periodontal diseases. Dermatol Clin. 2020;38(4):413-420. doi:10.1016/j.det.2020.05.002
2. Irshad M, Alam MK, Alawneh A, et al. Characterization and antimicrobial susceptibility of pathogens associated with periodontal abscess. Antibiotics (Basel). 2020;9(10):654. doi:10.3390/antibiotics9100654
3. Puletic M, Popovic B, Jankovic S, Brajovic G. Detection rates of periodontal bacteria and herpesviruses in different forms of periodontal disease. Microbiol Immunol. 2020;64(12):815-824. doi:10.1111/1348-0421.12857
4. Yousefi Y, Meldrum J, Jan AH. Periodontal abscess. In: StatPearls. StatPearls Publishing; August 20, 2021. http://www.ncbi.nlm.nih.gov/books/nbk560625/
5. Esmeili T, Lozada-Nur F, Epstein J. Common benign oral soft tissue masses. Dent Clin North Am. 2005;49(1):223-x. doi:10.1016/j.cden.2004.07.001
6. Rathva VJ. Traumatic fibroma of tongue. BMJ Case Rep. 2013;2013:bcr2012008220. doi:10.1136/bcr-2012-008220


