 A 3-month-old infant presented with a 4-week history of a symmetric skin eruption on her face, axillae, distal extremities, and external genitalia. The infant was otherwise healthy, although colicky since birth. She was exclusively breast-fed and had a good appetite. Voiding and stooling patterns were normal. Her growth was appropriate for age.
A 3-month-old infant presented with a 4-week history of a symmetric skin eruption on her face, axillae, distal extremities, and external genitalia. The infant was otherwise healthy, although colicky since birth. She was exclusively breast-fed and had a good appetite. Voiding and stooling patterns were normal. Her growth was appropriate for age.
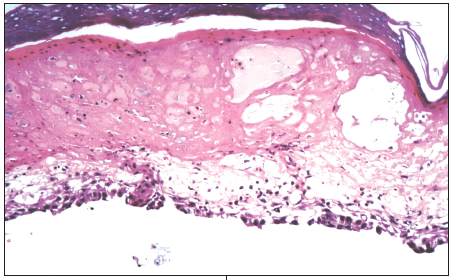
Cultures of the fluid from a representative lesion were negative for bacteria, yeast, and herpes simplex virus. Skin biopsy revealed areas of full-thickness necrosis and subepidermal splitting, as well as acanthosis with marked exocytosis and spongiosis. Histologic findings showed low numbers of leukocytes within the dermis. Direct immunofluorescence was negative for immunoglobulin and C3 deposits.
Which of these conditions is the likely diagnosis?
A. Mucocutaneous candidiasis
B. Zinc deficiency disorder
C. Necrolytic migratory erythema (glucagonoma)
D. Seborrheic dermatitis
(Answer and discussion begin on the next page.)
 Zinc deficiency disorder, or acrodermatitis enteropathica (AE), is a rare autosomal recessive disorder of zinc metabolism.1 It typically manifests after cessation of breast-feeding or earlier in formula-fed infants.2 AE classically presents as a clinical triad of bilateral, symmetric, acral, periorificial skin erosions; intractable diarrhea; and diffuse partial alopecia.3 Cutaneous features often precede the diarrhea by several weeks or months: discrete areas of moist erythema evolve into vesiculobullous or pustular lesions.4 Eventually, the lesions transform into erythematous plaques with silvery scale that resemble psoriasis.4 Weight loss, photophobia, apathy, alopecia, thrush, and paronychia secondary to Candida albicans infection can occur.4 Untreated patients with zinc deficiency can die of malnutrition and infection, primarily caused by immunologic defects (such as decreased natural killer cell activity, impaired delayed-type hypersensitivity, and thymic atrophy).3
Zinc deficiency disorder, or acrodermatitis enteropathica (AE), is a rare autosomal recessive disorder of zinc metabolism.1 It typically manifests after cessation of breast-feeding or earlier in formula-fed infants.2 AE classically presents as a clinical triad of bilateral, symmetric, acral, periorificial skin erosions; intractable diarrhea; and diffuse partial alopecia.3 Cutaneous features often precede the diarrhea by several weeks or months: discrete areas of moist erythema evolve into vesiculobullous or pustular lesions.4 Eventually, the lesions transform into erythematous plaques with silvery scale that resemble psoriasis.4 Weight loss, photophobia, apathy, alopecia, thrush, and paronychia secondary to Candida albicans infection can occur.4 Untreated patients with zinc deficiency can die of malnutrition and infection, primarily caused by immunologic defects (such as decreased natural killer cell activity, impaired delayed-type hypersensitivity, and thymic atrophy).3
An acquired form of zinc deficiency may develop in premature and term babies who are fed a zinc-deficient diet.4 The clinical picture mimics that of AE. Occasionally, human breast milk low in zinc can lead to deficiency in the exclusively breast-fed infant.4 The skin lesions in acquired deficiency are often mistaken for those of mucocutaneous candidiasis associated with immune deficiency.4
 Laboratory verification of zinc deficiency is the same for both the inherited (AE) and the acquired forms. A decrease in serum, hair, and urine zinc levels can be considered diagnostic of zinc deficiency. Serum zinc levels of less than 50 µg/dL are diagnostic and levels of 70 to 120 µg/dL are considered normal.5
Laboratory verification of zinc deficiency is the same for both the inherited (AE) and the acquired forms. A decrease in serum, hair, and urine zinc levels can be considered diagnostic of zinc deficiency. Serum zinc levels of less than 50 µg/dL are diagnostic and levels of 70 to 120 µg/dL are considered normal.5
Skin biopsy is not diagnostic. Histologic findings depend on the duration and clinical appearance of the lesions and may include hyperkeratosis, parakeratosis, intraepidermal pustules, spongiosis, acanthosis, and a mild polymorphic infiltrate in the upper dermis.5
 Treatment of infants with AE consists of oral zinc sulfate(, 5 mg/ kg/d in divided doses 2 or 3 times a day.5 Clinical response is rapid; apathy resolves within 24 hours, and skin lesions and diarrhea resolve within 7 to 14 days.4 In patients with refractory AE, determine the serum zinc level to confirm defective absorption. Affected patients can be treated with parenteral supplementation of zinc sulfate at dosages of 0.2 to 0.3 mg/kg/d.6
Treatment of infants with AE consists of oral zinc sulfate(, 5 mg/ kg/d in divided doses 2 or 3 times a day.5 Clinical response is rapid; apathy resolves within 24 hours, and skin lesions and diarrhea resolve within 7 to 14 days.4 In patients with refractory AE, determine the serum zinc level to confirm defective absorption. Affected patients can be treated with parenteral supplementation of zinc sulfate at dosages of 0.2 to 0.3 mg/kg/d.6
In acquired zinc deficiency disorders, continue treatment until the underlying disorder and clinical symptoms resolve. Patients with AE typically require lifetime zinc supplementation.
Consider the following conditions in the differential diagnosis:
• Mucocutaneous candidiasis presents in neonates as generalized eczematous and scaling skin. Typically, however, it presents as intense red patches and pustules accompanied by satellite lesions, usually within intertriginous regions. The lesions tend to become macerated. C albicans has been isolated from the skin and mucosal lesions in 20% of patients with AE.5 Nevertheless, this association represents a secondary infection in these areas--not a primary etiologic factor. The vesiculobullous eruptions of the periorificial and acral skin, cachexia, alopecia, and diarrhea of zinc deficiency help differentiate the conditions. In candidiasis, direct microscopic examination of scales scraped from the skin's surface demonstrates yeast forms.
• Necrolytic migratory erythema (glucagonoma) typically develops in adults who have overproduction of a2-glucagon by a pancreatic tumor. The clinicopathologic findings are identical to those of acquired zinc deficiency; however, the cutaneous manifestations are secondary to a deficiency of essential amino acids. Elevated serum levels of glucagon(, hyperglycemia, and hypoaminoacidemia are diagnostic.7
• Seborrheic dermatitis often develops within the first 12 weeks of life and spontaneously resolves by age 8 to 12 months. The diagnostic features include early onset, characteristic greasy skin lesions, and a predilection for the scalp and intertriginous areas. Unlike zinc deficiency disorders, seborrheic dermatitis spares the acral skin regions and mucous membranes.7


