Not Just Another Teenager With Rhinosinusitis
Case in Point
An Intriguing Diagnosis
A 14-year-old African American girl with a history of allergic rhinitis was admitted to our hospital with a 2-week history of severe frontal headaches. The headaches were associated with purulent rhinorrhea, fevers, and 2 syncopal episodes. Initial evaluation and workup in the emergency department revealed normal cerebrospinal fluid indexes, while a computed tomography (CT) scan showed opacification of the paranasal sinuses. A high-density material in the ethmoidal sinuses (Figure 1) was suggestive of allergic fungal sinusitis (AFS). Serologic testing revealed elevated immunoglobulin E titers (1,280 IU/mL). She was diagnosed with acute bacterial rhinosunusitis, was treated with clindamycin and ceftriaxone for 48 hours, and was discharged home on a 14-day course of oral amoxicillin-clavulanate.

Figure 1 — Computed tomography scan of the head shows high-density material within the left ethmoidal air cells and left frontal sinus, findings consistent with allergic fungal sinusitis.
Good clinical response was noted during her follow-up visit. However, 3 weeks later she returned to our emergency department with fever, headache, and neck stiffness. A head CT scan revealed a right subdural empyema and partial thrombosis of the superior sagittal sinus. She was started on intravenous ceftriaxone, vancomycin, metronidazole, and heparin infusion. Magnetic resonance imaging and magnetic resonance venography scans characterized the extent of the cavernous sinus thrombosis (Figure 2).

Figure 2 — Magnetic resonance venogram of the head shows an occlusive filling defect in the superior sagittal sinus.
The patient underwent endoscopic sinus surgery to address the presumed source of infection. Pus admixed with eosinophilic mucin was removed from the sinuses, with reported growth of fungal elements. She eventually required evacuation of the subdural empyema by neurosurgery. Her postoperative course was satisfactory, and she was discharged home with a 6-week course of antibiotics and enoxaparin.
ALLERGIC FUNGAL SINUSITIS: OVERVIEW
AFS is an important subtype of chronic sinusitis that presents in adolescents. It is distinguished from other types of chronic sinusitis by the presence of eosinophilic mucin that accumulates in the sinuses. In children especially, expansion of the sinus by accumulating mucin can result in facial dysmorphia, particularly proptosis. Up to 42% of children with AFS present with facial dysmorphia.1,2 Our patient did not have a disease burden sufficient to cause facial dysmorphia. Other presenting symptoms include nasal obstruction, anosmia, and rhinorrhea. African American children often present earlier and with more severe disease.3 Geographically, AFS is more prevalent in the U.S. Southeast and in other warm, humid climates worldwide.4
AFS is a noninvasive form of fungal sinusitis. Patients usually are immunocompetent, and up to 50% have comorbid asthma or allergic rhinitis.5 Patients demonstrate type I hypersensitivity to dematiaceous fungi, including Aspergillus species.6 Fungi can be found in eosinophilic mucin that accumulates in the paranasal sinuses.
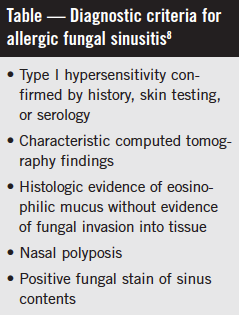
The diagnosis of AFS is suspected in patients with characteristic findings on CT scans, namely asymmetric, heterogenous opacification and bony attenuation, and expansion of the paranasal sinuses (Table).7,8
The treatment of AFS typically includes endoscopic sinus surgery to remove eosinophilic mucin. Saline irrigations and topical and systemic corticosteroids are used to decrease the inflammation. Consultation with otolaryngology is recommended.
Infectious complications from AFS are rare. However, this patient had a superimposed acute bacterial sinusitis that was the likely cause of her intracranial complications. Bacterial sinusitis can occur in patients with AFS due to obstruction of the sinus outflow tracts.9 Complicated acute bacterial sinusitis refers to infection that has spread beyond the paranasal sinuses.10 Periorbital cellulitis is the most common complication of acute bacterial rhinosinusitis. Epidural empyema is the most common intracranial complication, followed by meningitis, intracranial abscess, and, less commonly, cerebral sinus thrombosis, as in our case.11
TAKE-HOME MESSAGE
This case represents an unusual constellation of sinonasal pathology. Pediatricians should suspect AFS in patients with characteristic imaging findings and should recognize intracranial complications in patients with acute bacterial sinusitis.
REFERENCES:
1. McClay JE, Marple B, Kapadia L, et al. Clinical presentation of allergic fungal sinusitis in children. Laryngoscope. 2002;112(3):565-569.
2. Wise SK, Venkatraman G, Wise JC, DelGaudio JM. Ethnic and gender differences in bone erosion in allergic fungal sinusitis. Am J Rhinol. 2004;18(6):397-404.
3. Wise SK, Ghegan MD, Gorham E, Schlosser RJ. Socioeconomic factors in the diagnosis of allergic fungal rhinosinusitis. Otolaryngol Head Neck Surg. 2008;138(1):38-42.
4. Ferguson BJ, Barnes L, Bernstein JM, et al. Geographic variation in allergic fungal rhinosinusitis. Otolaryngol Clin North Am. 2000;33(2):441-449.
5. Manning SC, Holman M. Further evidence for allergic pathophysiology in allergic fungal sinusitis. Laryngoscope. 1998;108(10):1485-1496.
6. Katzenstein AL, Sale SR, Greenberger PA. Allergic Aspergillus sinusitis: a newly recognized form of sinusitis. J Allergy Clin Immunol. 1983;72(1):89-93.
7. Meltzer EO, Hamilos DL, Hadley JA, et al. Rhinosinusitis: establishing definitions for clinical research and patient care. J Allergy Clin Immunol. 2004;114(6 suppl):155-212.
8. Bent JP III, Kuhn FA. Diagnosis of allergic fungal sinusitis. Otolaryngol Head Neck Surg. 1994;
111(5):580-588.
9. Sacks PL IV, Harvey RJ, Rimmer J, Gallagher RM, Sacks R. Antifungal therapy in the treatment of chronic rhinosinusitis: a meta-analysis. Am J Rhinol Allergy. 2012;26(2):141-147.
10. Bozeman S, deShazo R, Stringer S, Wright L. Complications of allergic fungal sinusitis. Am J Med. 2011;124(4):359-368.
11. DeMuri GP, Wald ER. Complications of acute bacterial sinusitis in children. Pediatr Infect Dis J. 2011:30(8):701-702.


