Neonatal Stroke Induced by Factor V Leiden Mutation
A meconium-stained, nonvigorous girl was born at 41 weeks of gestation via normal, spontaneous vaginal delivery to a 30-year-old, gravida 1, para 1 mother. The maternal history and prenatal laboratory test results were unremarkable. Meconium suction from the neonate’s airway and positive pressure ventilation for 30 seconds were provided according to the American Academy of Pediatrics/American Heart Association Neonatal Resuscitation Program guideline.
The girl’s Apgar score was 4 at 1 minute and 8 at 5 minutes. She was transferred to the neonatal intensive care unit (NICU) due to delayed fetal-to-neonatal transition. In the NICU, the patient’s vital signs were stable. Oxygenation at 4 L/min was administered via a high-flow nasal cannula for 6 hours to reduce desaturation. The results of chest radiographs and a complete blood count were normal. Antibiotics were started pending blood culture results.
At 24 hours of age, the newborn developed twitching on the left face, lasting 60 seconds, with eye blinking and jerking arm movements. A loading dose and a maintenance dose of phenobarbital were given. Results of cerebrospinal fluid studies were unremarkable.
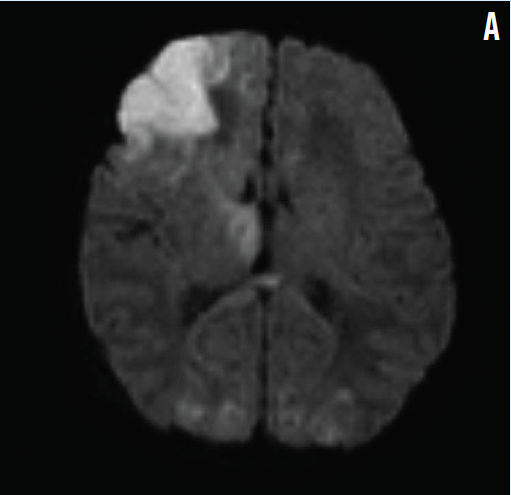
At 40 hours of age, diffusion-weighted magnetic resonance imaging (MRI) revealed restricted diffusion in the right frontal lobe cortex, basal ganglia, thalamus, and occipital lobes representing an ischemic infarct (Figure A). Electroencephalography demonstrated localized sharp-wave activity in the right temporal area.
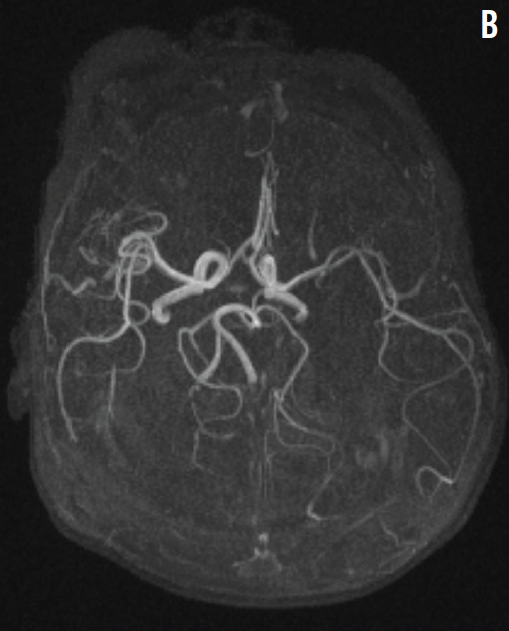
The results of magnetic resonance angiography (MRA) showed no vascular malformation (Figure B), but contrast enhancement in the right frontal lobe suggested arterial ischemic stroke.
Further evaluation with echocardiography, chromosome analysis, newborn screening tests, and tests for levels of serum lactic acid, plasma homocysteine, plasma amino acids, and urine organic acids revealed normal results. Hematologic evaluation revealed normal results for prothrombin time, partial thromboplastin time, international normalized ratio, antithrombin III activity, and protein C and S activity. Results of a factor V DNA genetic screening test were positive for heterozygous factor V Leiden mutation R506Q.
Discussion
Ischemic perinatal stroke occurs in 1 of 2,300 to 5,000 live births and is defined as cerebral injury of vascular origin occurring between 20 weeks of gestation and 28 days of postnatal life.1 The etiology is multifactorial and often is difficult to identify.1-3 Pathophysiologic mechanisms involved in ischemic perinatal stroke include emboli, cerebral vascular malformation, and disturbed hemostasis.1,4-6
In our patient, MRI results suggested an arterial origin of the frontal ischemic stroke. Normal echocardiography results ruled out congenital heart disease. No central nervous system defects or vascular malformations were seen on MRI and MRA images. Normal newborn screening test results ruled out homocysteinemia and other inborn errors of metabolism. The patient had no evidence of hypoxic ischemic encephalopathy.
The etiology of arterial ischemic stroke in this infant was attributed to factor V Leiden heterozygous mutation. To our knowledge, 6 cases of perinatal stroke have been reported in association with factor V Leiden mutation, and all 6 involved hemorrhagic infarction.7-9
Treatment and Prognosis
Supportive care is the suggested treatment for neonatal ischemic stroke, which we provided for this newborn. Withholding anticoagulation therapy is reasonable if a cardiac or embolic origin has been excluded.1,3 Long-term neurodevelopmental outcomes are normal in 19% to 33% of cases. However, neonatal stroke is a leading cause of hemiplegia (30% of cases); deficits in language, vision, and cognition occur in 20% to 60% of cases and evolve over years, making multispecialty follow-up necessary.1,2,10 Neonatal stroke rarely recurs.1,3
Our patient had normal cognitive and motor development at follow-up at 15 months of age.
Factor V Leiden mutation causing neonatal stroke, while rare, should be considered in the broad differential diagnosis of neonatal focal seizures.
References
- Raju TN, Nelson KB, Ferriero D, Lynch JK; NICHD-NINDS Perinatal Stroke Workshop Participants. Ischemic perinatal stroke: summary of a workshop sponsored by the National Institute of Child Health and Human Development and the National Institute of Neurological Disorders and Stroke. Pediatrics. 2007;120(3):609-616.
- Nelson KB, Lynch JK Stroke in newborn infants. Lancet Neurol. 2004;3(3):150-158.
- Kirton A, Armstrong-Wells J, Chang T, et al; International Pediatric Stroke Study Investigators. Symptomatic neonatal arterial ischemic stroke: the International Pediatric Stroke Study. Pediatrics. 2011;128(6):e1402-e1410.
- Barmada MA, Moossy J, Shuman RM. Cerebral infarcts with arterial occlusion in neonates. Ann Neurol. 1979;6(6):495-502.
- Ment LR, Duncan CC, Ehrenkranz RA. Perinatal cerebral infarction. Ann Neurol. 1984;16(5):559-568.
- Lynch JK, Nelson KB, Curry CJ, Grether JK. Cerebrovascular disorders in children with the factor V Leiden mutation. J Child Neurol. 2001;16(10):735-744.
- Thorarensen O, Ryan S, Hunter J, Younkin DP. Factor V Leiden mutation: an unrecognized cause of hemiplegic cerebral palsy, neonatal stroke, and placental thrombosis. Ann Neurol. 1997;42(3):372-375.
- Varelas PN, Sleight BJ, Rinder HM, Sze G, Ment LR. Stroke in a neonate heterozygous for factor V Leiden. Pediatr Neurol. 1998;18(3):262-264.
- Verdu A, Cazorla MR, Moreno JC, Casado LF. Prenatal stroke in a neonate heterozygous for factor V Leiden mutation. Brain Dev. 2005;27(6):451-454.
- Sreenan C, Bhargava R, Robertson CMT. Cerebral infarction in the term newborn: clinical presentation and long-term outcome. J Pediatr. 2000;137(3):351-355.


