A Collection of Cysts
Lymphangioma Circumscriptum With Secondary Cellulitis
Micael L. Sternberg, MD, and Nate Lisen Bee, MS
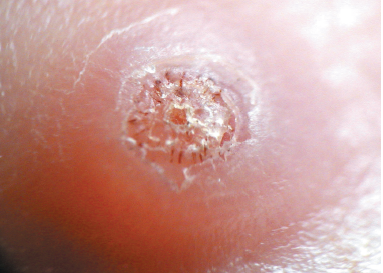
A 6-year-old boy had redness and pain of skin on his left upper abdomen for the past 3 days. Physical examination revealed a large cluster of vesicles with underlying erythema and mild warmth.
History. The patient’s mother stated that the lesion had been present for 5 years, that it had been diagnosed as lymphangioma circumscriptum by a dermatologist, and that excision was pending. Secondary cellulitis of the existing lesion was considered, and an oral antibiotic was prescribed. At follow-up, signs of infection had cleared.

Discussion. Lymphangiomas, which make up about 4% of all vascular tumors and 26% of benign vascular tumors in children, are divided into 4 main types: lymphangioma circumscriptum, cavernous lymphangioma, cystic hygroma, and benign lymphangioendothelioma.1 Lymphangioma circumscriptum is a rare type caused by dilation of subcutaneous lymphatic cisterns, which leads to outpouchings that protrude through the skin and form vesicles.2 Half of cases present at birth, and 90% present by age 2 years.3
Clinically, the disorder can be described as clusters of small (usually 1- to 2-mm) translucent vesicles; hemorrhage in and around the vesicles may cause the lesions to appear pink, red, or black.2 The lesions can occur anywhere on the skin or mucous membranes, but they most commonly develop on the proximal extremities, trunk, axillae, and buttocks.1 The differential diagnosis can include warts, molluscum contagiosum, hemangioma, angiokeratoma, lymphangioendothelioma, lymphangiectasis, metastatic carcinoma of the skin, herpes simplex, herpes zoster, dermatitis herpetiformis, and malignant melanoma.2,3
Treatment. Cosmesis, pain, swelling, and recurrent cellulitis could all warrant treatment.3 Options include cryotherapy, laser therapy, sclerosing agents, and liposuction, but surgical resection using MRI to obtain adequate margins is preferred.2
REFERENCES:
- Heller M, Mengden S. Lymphangioma circumscriptum. Dermatol Online J. 2008;14(5):27.
- Mordehai J, Kurzbart E, Shinhar D, et al. Lymphangioma circumscriptum. Pediatr Surg Int. 1998;13(2-3):208-210.
- Patel GA, Schwartz RA. Cutaneous lymphangioma circumscriptum: frog spawn on the skin. Int J Dermatol. 2009;48(12):1290-1295.
Sebaceous Cyst
Les Trope, MD, Hillel Trope, MD, and Shlomo Trope, MD
A 36-year-old man had a painless swelling on the dorsum of the scalp that had been present for many years. An increase in the size of the lesion prompted the man to seek medical evaluation. Differential diagnosis included lipoma and kerion (a condition associated with tinea infections).

The well-demarcated edge of the lesion and results of a transillumination test showing fluid within the lesion ruled out a lipoma. The absence of dryness and scaliness excluded a kerion; moreover, kerions are flat. The punctum on this lesion contributed to its identification as a sebaceous cyst. Also called pilar cyst, or wen, a sebaceous cyst is a benign, slow-growing mass that contains keratinous and/or follicular materials. This nontender cyst typically forms on the scalp but may occur on the ears, face, back, or scrotum.
Treatment is surgical for a sebaceous cyst of this size.
Epidermoid Cyst of the Testis
Joseph Anderson, MD, and Nathan C. Birch, MD
A 25-year-old man sought evaluation of a painless, palpable, left testicular mass that had been present for more than 1 year. There was no personal or family history of cryptorchidism or malignancy. A circumscribed mass was palpated within the anterior superior pole of the left testis.
Initial laboratory test results were within normal limits. An ultrasonogram revealed a 1.6 cm × 1.2 cm × 1.2 cm cystic structure with alternating hypoechogenicity and hyperechogenicity (Figure 1) that strongly suggested an epidermoid cyst; however, a carcinoma could not be ruled out. A period of monitoring with ultrasonographic examinations was observed for several months. This patient subsequently underwent a partial orchiectomy; although a benign cyst was suspected, the surgeon opted for this procedure to exclude intratubular germ cell neoplasia.

Pathologic examination revealed a well-circumscribed, white-tan, laminated lesion within unremarkable, red-brown testicular parenchyma (Figure 2). The largest dimension of the mass was 1.6 cm. Microscopic examination confirmed the diagnosis of a benign epidermoid cyst.
Epidermoid cysts comprise 1% of testicular masses.1 These well-circumscribed, solid masses, which most often occur in the second to fourth decades of life, are not associated with distant metastases or local recurrence.1-3 The cyst is composed of a fibrous wall lined with squamous epithelium and filled with keratin debris. The layering of this debris imparts the classic “onion skin” or “target” appearance on an ultrasonogram.4
The differential diagnosis includes a dermoid cyst, mature teratoma, and germ cell neoplasm.5 Germ cell tumor can be ruled out by histologic examination. Preoperative ultrasonographic evaluation that strongly suggests an epidermoid cyst can direct the therapeutic course toward lesion enucleation, which is a more conservative treatment than a radical orchiectomy. The patient’s recovery was uneventful and complete.
References:
- Shah KH, Maxted WC, Chun B. Epidermoid cysts of the testis: a report of three cases and an analysis of 141 cases from the world literature. Cancer. 1981;47(3):577-582.
- Malek RS, Rosen JS, Farrow GM. Epidermoid cysts of the testis: a critical analysis. Br J Urol. 1986;58(1):55-59.
- Dieckmann KP, Loy V. Epidermoid cyst of the testis: a review of clinical and histogenetic consideratrions. Br J Urol. 1994;73(4):436-441.
- Langer JE, Ramchandani P, Siegelman ES, Banner MP. Epidermoid cysts of the testicle: sonographic and MR imaging features. AJR Am J Roentgenol. 1999;173(5):1295-1299.
- Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 2nd ed. New York, NY: Churchill Livingstone; 2000:810-811.
Synovial Cysts
Dmitry Shtrambrand, MD
Over the past year, asymptomatic wart-like nodules had slowly developed on the fingers of both hands of a 57-year-old woman. During that time, she also had noticed increasing stiffness and pain in her hands in the evening. She had hypertension, which was treated with an angiotensin-converting enzyme inhibitor.

No drainage from the nodules was evident. Proximal and distal interphalangeal joint changes were noted, which were consistent with osteoarthritis.
The synovial fluid aspirated by a rheumatologist was characteristic of osteoarthritis, with a white blood cell count of 750/µL and high viscosity.
Erosive osteoarthritis nodules are basically synovial cysts that extend outside the joints. Synovial cysts should not be confused with Heberden or Bouchard nodes, which represent joint widening or deformity.
The patient was treated with oral methotrexate and corticosteroid injection into the cysts. At the 3-month follow-up visit, the nodules had not resolved; however, the treatment had alleviated the stiffness and pain in the patient’s hands, and no new nodules had appeared in the interim.
Peroneal Ganglion
Alexander K.C. Leung, MD, and Justine H.S. Fong, MD
A 7-year-old boy presented with an asymptomatic cystic lesion on the lateral aspect of the left ankle of 4 months’ duration. There was no history of trauma. The mass fluctuated in size; it was smaller when the child was recumbent and larger when the child was upright.

Physical examination. Musculoskeletal examination of the spine, upper extremities, and lower extremities was entirely unremarkable, except for a tensely cystic mass over the lateral aspect of the left ankle just inferior to the lateral malleolus.
The mass measured 3 cm × 1.5 cm. It nicely transilluminated when an otoscope was placed over its top. The mass did not change in size when the peroneal tendons were stressed or when the foot moved through a full range of motion. A sonogram of the left ankle confirmed the presence of a lobulated elongated cyst of 3 cm × 1.5 cm.
The patient received a diagnosis of a peroneal ganglion.
Discussion. This benign, fluid-filled cyst results from either herniation of the synovium through a defect in a joint or myxomatous degeneration of the connective tissue close to a joint or tendon.
The lesion is typically connected to the underlying joint capsule or tendon sheath by a stalk that may be tortuous. Transillumination with an otoscope is an easy way to establish the diagnosis. Ultrasonography can help to better define the mass.
The lesion is usually asymptomatic but may become tender as it expands or when it is impacted. Sites of predilection include the dorsum of the wrist, dorsum of the foot, and the ankle. In children, ganglia are usually benign and tend to disappear over time.
Treatment. Operative excision is recommended if the lesion is painful, unsightly, interferes with normal tendon function, or rapidly increases in size.
Because none of the indications were present in this patient, therapy was conservative.
Calcified Splenic Cyst
Riad O. El Fakih, MD, Wissam A. Saliba, MD, and Rami A. Mortada, MD
A 38-year-old man found lying on the floor in his home was hospitalized because of alcohol intoxication. A chest radiograph showed a large calcified lesion in the left upper abdomen (Figure 1). A CT scan with intravenous contrast revealed a large, well-defined, cystic mass with mural calcification in the spleen (Figure 2)

The CT findings were not consistent with a vascular malformation or echinococcal cyst—specifically, the mass was sharply demarcated, unilocular without septations, and round with a thin wall and attenuation similar to water. Urine Histoplasma antigen test results were negative.
Laboratory testing. The patient underwent CT-guided aspiration of the cyst, and the fluid was cultured and examined under microscopy. Culture, cytology, and Gram stain results were negative, and no parasitic elements were identified under microscopy. Based on these results and the lack of a patient history of pancreatitis, traumatic calcified splenic cyst was diagnosed.

Discussion. Calcified splenic cysts most often occur in patients who are prone to recurrent blunt abdominal trauma, such as persons with alcoholism. However, it is a diagnosis of exclusion; more common, treatable causes of splenic masses must be ruled out first. n


