Advance Directives Revisited
Key words: Advance directives, end-of-life care, advance care planning, living will, healthcare proxy, durable power of attorney, decision-making capacity.
__________________________________________________________________________________________
While advance directives are now a recognized component of medical care and patients are urged to have these prepared and available for when the need arises, many physicians fail to take sufficient time and make a significant effort to review the content of these documents with their patients, assuming that this important aspect of medical care is handled between patients and their attorneys. Furthermore, although there is a wealth of preprinted and online documents on advance directives available to the consumer, and patients in many cases merely check off or circle which paragraph or answer choice they desire from a list of several options, terminology may at times be difficult to interpret. The end result may leave physicians finding themselves at odds with family members or healthcare proxies as to what the patient truly intended prior to losing his or her decision-making capacity.
To avoid such conflicts, it is important to discuss what is contained within an existing advance directive with any patient who still has the capacity to make his or her own decisions, enabling modifications to be made with regard to the patient’s current wishes and circumstances. Clearly, physicians must be comfortable in first determining whether their patient has the capacity to continue to make such decisions. In addition, caution is advised so that patients are not judged to lack capacity merely because of an inaccurate diagnosis in the chart, such as wrongly being labeled as having dementia or having hearing deficits, expressive aphasias, or other medical conditions that do not impair decision-making capacity but merely complicate communication ability. What follows are two cases that illustrate some of the issues that may arise during end-of-life care, even with the presence of an advance directive. We also review the history of advance directives; discuss patient autonomy and capacity; outline some challenges with regard to creating and executing advance directives; and review the terminology used in advance directives, during advance care planning discussions, and with regard to end-of-life care.
Case 1
An 81-year-old woman was admitted to the intensive care unit after falling from a standing position, resulting in bilateral subarachnoid hemorrhages and a left maxillary bone fracture. The exact cause of her fall could not be ascertained. The patient required initial intubation and was placed on a ventilator due to trouble with maintaining proper oxygenation.
The patient had an advance directive indicating that she did not want any invasive measures in the setting of cardiac arrest. It also stated, “If I have a terminal condition and death is imminent, I do not want any life-prolonging treatment, including intravenous nutrition or other medical treatment.”
Despite her physician’s view that it was too early to decide whether the patient was in a terminal state and “death was imminent”—in fact, the physician felt that she might even be able to return to her baseline functioning—the family asked that all treatment be withdrawn. They expressed that this was her wish in her advance directive, and they wanted to honor it. After considerable discussion, the physician agreed to the family’s wishes, and the patient died shortly after being taken off mechanical ventilation.
Case 2
An 86-year-old woman was admitted to the hospital after falling and sustaining a fractured femur. She had a stroke several years earlier that left her with an expressive aphasia. She had a poor caloric intake that caused her to lose weight over the previous few months. During the patient’s current admission, her in-hospital healthcare providers labeled her as “demented” after not being able to communicate with her, and they were in contact with her family regarding desired options for care. Her physician judged her as not being able to eat sufficiently, and her family insisted on having a feeding tube placed.
Upon further review, an advance directive completed by the patient decades earlier was discovered, but there was no information available as to whether it had ever been reevaluated by the patient since its execution. Her advance directive stated that she did not want to be fed by artificial means if she had “an incurable injury, disease, or illness certified to be a terminal condition by two physicians who have personally examined me, one of whom shall be my attending physician, and the physicians have determined that my death is imminent and will occur whether or not life-sustaining procedures are utilized and where the application of such procedures would serve to only artificially prolong the dying process.” What made things even more complicated was that the geriatric consultant was able to use hand signs to communicate with the patient and believed that she was fully able to comprehend what was being asked of her, as she responded appropriately to questioning and demonstrated the capacity to make her own decisions. Upon further questioning by the geriatric consultant, it was clear that the patient was adamant about not wanting a feeding tube inserted.
Because the patient did not meet the criteria delineated by her advance directive at the time of her admission, and had she been unable to express her own wishes, her family’s desires for a feeding tube to be inserted would have been honored by her physicians given no other direction in the available advance directive. After careful review and discussion, however, the patient’s own wishes not to have a feeding tube were honored. The geriatric consultant demonstrated the patient’s ability to comprehend what was being asked and to respond appropriately, and other healthcare professionals were consistent in their interpretation of the patient’s wishes at this time. Her family eventually agreed with her decision and stopped pressing for an artificial feeding tube to be inserted.
Discussion
There are two major types of advance directives: a living will and a durable power of attorney, the latter of which is called a healthcare proxy or healthcare power of attorney when it covers healthcare matters. Table 1 provides definitions of this terminology and other terms included in advance directives and used during end-of-life discussions.1-5 A living will is a legally executed document that specifically delineates what forms of medical treatment are preferred if an individual loses decision-making capacity. A living will can have specific treatments mentioned or can give general direction. Commonly used terms found in living wills include irreversible illness, incurable disease, and imminent death, among others.2 Some living wills give direction regarding end-of-life care measures, such as resuscitation, desired forms of hydration and feeding, use of antibiotics, and use of ventilators.
A durable power of attorney designates a specific individual to act on a person’s behalf once that person becomes unable to act on his or her own behalf. It may be general or limited.3 When a durable power of attorney is limited, the designated power of attorney, who is also known as the designated proxy, only acts on the person’s behalf for certain events, such as managing his or her finances, handling legal matters, or making healthcare decisions. In the event healthcare decisions are covered by the durable power of attorney, this legal document is often referred to as the durable attorney for healthcare. Through this document, the designated proxy is enabled to make healthcare decisions if the patient loses the capacity to make an informed decision or cannot make his or her wishes known to others. The designated proxy has the same rights as the patient to express what treatments the patient may or may not desire at a specific point in the patient’s illness.


History of Advance Directives
End-of-life issues have long been the focus of intense societal debate as providers, medical ethicists, policy makers, legislators, and the public have considered essential questions concerning patient autonomy, quality of life, and withdrawal of life-sustaining treatments. In 1914, the first law was established that required a patient’s consent for invasive medical procedures based on the right of self-determination.1 Physicians continued to make most patient care decisions, however, and focused primarily on cure or comfort. The consumer rights movement in the 1960s began to push for additional options, such as hospice programs, to free terminally ill patients from aggressive and ultimately futile life-sustaining treatment.1
In 1967, attorney Luis Kutner was credited as being the first person to suggest that a “living will” be created. It was his intention to honor “the rights of dying people to control decisions about their own medical care.”6 In 1968, Florida was the first state legislature to debate a bill that would enable patients to make decisions regarding their use of life-sustaining equipment at some future time. While this bill failed to pass initially, its physician sponsor, Walter F. Sackett, reintroduced the bill in 1973 only to have it once again defeated. A similar bill was introduced in California but was also defeated in 1974. Upon reintroduction in 1976 by its sponsor, Barry Keene, the California Natural Death Act of 1976 was passed and California became the first state in the nation to legalize living wills.2 That same year, the New Jersey Supreme Court was the first state to validate the use of advance directives.2 Joe Quinlan requested to the court that he legally be recognized as having the right to make binding healthcare decisions for his daughter, Karen Ann Quinlan. In a decision by Chief Justice Robert Hughes, the following judicial principles were put forth2:
1. Patients who are judged to be mentally unable to make treatment decisions may have someone else exercise their rights for them.
2. Decisions that may cause a mentally incompetent patient to die are best made by the patient’s family members with the input of the patient’s physicians.
3. End-of-life decisions should take into consideration both the invasiveness of the proposed treatment and the patient’s likelihood of recovery.
4. Patients have the right to refuse treatment, even if this refusal might lead to their death.
As a result of this case, Karen Ann Quinlan was gradually weaned from mechanical ventilation. By 1977, 43 state legislatures were considering legalizing living wills, whereas seven had already approved their use. By 1992, however, all 50 states and the District of Columbia had passed legislation to legalize the use of advance directives in one form or another.2
In 1978, the federal government formed the President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research.7 This commission worked until 1983 to address the difficult topics of defining death, what it meant to have a “permanent loss of consciousness,” issues of withholding and withdrawing life-sustaining treatments, and the importance of advance directives. The Uniform Determination of Death Act was based on the commission’s 1981 report Defining Death.7
In 1990, the US Supreme Court agreed to hear a case regarding the legality of advance directives.8 In the case, Cruzan v Director, the family of Nancy Cruzan petitioned to discontinue percutaneous gastrostomy tube feedings. The Court decided in favor of the individual’s right to refuse treatment, even though it was essential to sustain life. No specific decision was made regarding this specific case, however, and the opinion was referred back to the Missouri Supreme Court for action. It was eventually agreed that there was a prior verbal advance directive that supported the refusal of medical treatment, and tube feedings were, in fact, able to be discontinued.8
In 1991, the US House of Representatives enacted the Patient Self-Determination Act, which stipulated that all hospitals receiving Medicare or Medicaid reimbursement must ascertain whether a patient has or wishes to have an advance directive.2 This act did not create or legalize advance directives but validated that they exist in all states in the nation.
In 1993, the Uniform Health-Care Decisions Act (UHCDA) attempted to deal with both the broader problem of healthcare decision-making and the narrower problem of who is able to decide when to withdraw treatment and allow a patient to die.1 The act applies to healthcare decisions for adults and emancipated minors. In brief, it states that any adult or emancipated minor with the mental capacity to make decisions may give oral or written instruction to a healthcare provider that remains in force even after the individual loses capacity.1
In 1996, the US military adopted an advance directive provision that stated that advance directives executed by members of the armed forces are “exempt from any requirement of form, substance, formality, or recording that is provided for advance medical directives under the laws of a state.”9 It also stated that these directives “shall be given the same legal effect as an advance medical directive prepared and executed in accordance with the laws of the state concerned.” Therefore, if a document is a Military Power of Attorney, it will be honored even if it does not meet the standards of the state in which it is executed (eg, not being in a particular format or lacking the required witnesses).
Patient Autonomy and Capacity
Patient autonomy and individual choice are core values in Western bioethics and remain important components of end-of-life decision-making.10 As such, it is imperative that healthcare providers honor patient preferences for end-of-life care, even if they do not agree with them, provided these preferences fall within the range of accepted medical practice. Most ethicists agree that the principle of patient autonomy centers around protecting and promoting the patient’s ability to make informed decisions.10
In medicine, capacity is the clinical determination that addresses the integrity of mental function and the ability to make decisions (see Table 1).11 Its determination depends on the decision, the skills necessary to make the decision, and the degree to which illness impairs these skills. Patients are legally presumed to have the capacity to consent to or refuse medical care unless clinical data suggest otherwise. Patients must be given the information that is relevant to making an informed decision about their treatment. This should include the nature of the patient’s condition, the nature and purpose of the proposed treatment, and the risks and benefits of the proposed treatment and of alternative treatments (if available), including the option of no treatment at all. Care providers should not provide patients with this information in a written document or preprinted form and assume the information is well understood by patients. In addition, evaluators should ask a physician responsible for the patient’s care to disclose the relevant information again in the evaluator’s presence or the evaluator should undertake such disclosure.
In the event that the patient’s mental state fluctuates, impairing his or her level of capacity, a decision that a patient lacks capacity should be deferred whenever possible until at least two evaluations have been performed at different times. Collateral informants, such as family members and nursing staff, may be helpful in assessing capacity, and documentation on who was present when the evaluation took place is recommended. While patients should generally be informed of the purpose of the evaluation, they need not give explicit consent for the assessment to occur.
Preserving Patient Autonomy With Advance Directives  Healthcare advances have resulted in longer life expectancies, even among persons with chronic diseases, resulting in many more people relying on others to help them make everyday decisions. Eventually, many of these people become completely incapable of making any decisions on their own, whether due to cognitive decline or for a variety of other reasons. Advance care planning, culminating in the development of an advance directive, is essential to preserving patient autonomy by ensuring these persons’ wishes are maintained when they lose the ability to make decisions or express their wishes.
Healthcare advances have resulted in longer life expectancies, even among persons with chronic diseases, resulting in many more people relying on others to help them make everyday decisions. Eventually, many of these people become completely incapable of making any decisions on their own, whether due to cognitive decline or for a variety of other reasons. Advance care planning, culminating in the development of an advance directive, is essential to preserving patient autonomy by ensuring these persons’ wishes are maintained when they lose the ability to make decisions or express their wishes.
Clinicians should keep in mind that advance directives are almost always used toward the end of life, after patients have lost the capacity to make their own decisions. They are not intended to be a substitution for discussing care options with a person who retains the capacity to make decisions for himself or herself. Because advance directives communicate a patient’s preferences, it is important for all persons who will be involved in the patient’s care at the end of life to communicate effectively so that they understand those preferences. It is also important for the patient’s advance directive to remain as current as possible, ensuring the patient’s true wishes are carried out. Table 2 provides some strategies for ensuring proper communication between all concerned parties and for appropriate handling of a patient’s advance directive to ensure the patient’s wishes are honored.1
Challenges to Creating and Implementing Advance Directives 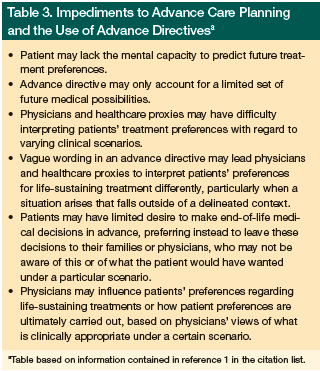 Despite advance directives being widely recognized as important documentation, four out of every five adults in the United States do not have an advance directive.6 Some patients are unaware of the need for advance directives or are less inclined to complete advance directives or engage in advance care planning.12-15 The latter group, for instance, may consist of individuals who have been disenfranchised and those with less trust in the medical care system. Studies also show that for many racial/ethnic groups, autonomy is not always empowering, information about bad news may not be invited, and appointed decision-makers may be an unacceptable decision-making mechanism.12-15 Some of the other numerous impediments to advance care planning and the use of advance directives are outlined in Table 3.
Despite advance directives being widely recognized as important documentation, four out of every five adults in the United States do not have an advance directive.6 Some patients are unaware of the need for advance directives or are less inclined to complete advance directives or engage in advance care planning.12-15 The latter group, for instance, may consist of individuals who have been disenfranchised and those with less trust in the medical care system. Studies also show that for many racial/ethnic groups, autonomy is not always empowering, information about bad news may not be invited, and appointed decision-makers may be an unacceptable decision-making mechanism.12-15 Some of the other numerous impediments to advance care planning and the use of advance directives are outlined in Table 3.
In one study, which took place in the primary care setting, the investigators reported that a discussion about and distribution of advance directive forms resulted in a 45% return rate.16 Older patient age (P=.001), longer length of time as a patient in the practice (P=.039), less education (P=.025), and physician provider (P=.002) were associated with higher completion rates. This study shows that physicians can play an important role in getting patients to complete advance directives; however, merely completing forms may not be sufficient if the patient’s true wishes remain open to interpretation. Therefore, if physicians distribute and receive advance directives, they should ask to see the forms after they are completed and review their contents with their patients to ensure that there is no ambiguity.
Another study evaluated physician education (oral and written) and physician and patient prompts to discuss advance directives.17 The intervention resulted in a 20-fold increase (95% confidence interval, 10.4-47.8) in the odds of creating a new advance directive. Physicians reported barriers of time and an unwillingness to press discussions with patients as ongoing obstacles.
Even when advance directives exist, a variety of problems may arise. For example, there might be mistrust or disagreement over a patient’s prognosis. Other times, conflict may occur when families desire life-sustaining treatment for persons with a compromised health state for which providers find such treatment to be inappropriate or are even at odds with what is listed in an advance directive. These situations are most commonly the result of poor early patient-provider communication and vague terminology in available documents, but they may also be the result of philosophical or religious differences that result in providers implementing what may be perceived as “futile” care. In response to such scenarios, providers may attempt to minimize the influence of patient and/or family preferences on care decisions; however, this approach is not without potential repercussions. Clinicians risk overstepping their authority and facing legal consequences if they act without consent when there is no medical urgency.
A patient’s healthcare surrogate/proxy should fully participate in the decision process whenever possible. In certain situations, this individual must make a best-interest decision on the patient’s behalf; thus, his or her primary role is to support patient autonomy by attempting to work with clinicians so that medical care can achieve the goals of the patient under any clinical circumstances. When conflict arises with regard to interpreting a patient’s perceived goals, physicians would be wise to work with their local risk management departments and seek legal counsel as to the best course of action in a given circumstance.
To prevent conflicts, providers, patients, and families should make the utmost effort to capture patients’ current wishes with regard to their care. It is also important that a discussion is held between the patient, the physician, and his or her family/future proxy, if appropriate, while the patient still has the capacity to ensure that any ambiguity is explained and all persons are clear with regard to the wishes delineated. While there is no specific “billing code” that physicians can use to bill for the time it takes to review an advance directive with a patient and his of her family/
future proxy, clearly this discussion is necessary and should be incorporated into every patient’s ongoing medical care. When having these discussions, it is essential for healthcare providers to use clear, consistent terminology, as variations in the terminology used to discuss advance care planning, advance directives, and end-of-life care can lead to misunderstandings. Each state regulates use of advance directives differently, and statutes enacted in one state may use terms and definitions that are different from those contained in advance directives completed in another state. Table 1 outlines the terminology used as part of the UHCDA and the Patient Self-Determination Act.1,5
Case Analysis
Returning to the patient in case 1, who had an advance directive that stated the following: “If I have a terminal condition and death is imminent, I do not want any life prolonging treatment, including intravenous nutrition or other medical treatment.” As previously stated and exemplified here, certain terminology may lead to misinterpretations that may not truly represent a patient’s wishes under certain circumstances. As long as the patient has the capacity to make an informed decision, advance directives can be altered at any time by the patient or even disregarded upon request. What is clear is that whatever is included in one’s advance directive should be able to be interpreted in a similar way by all physicians, healthcare administrators, social workers, nurses, and family members/surrogates/proxies.
This case illustrates the problem that may result when trying to interpret a patient’s prior wishes despite the presence of an advance directive form. Unfortunately, the terminology used in this case, as in many other advance directives, may be open to varying degrees of interpretation. Our patient no longer had the capacity to make an informed decision for herself or to express her wishes regarding certain life-sustaining measures when admitted to the hospital. It should also be noted that the advance directive form used was not specifically written for our patient but rather was a preprinted form for individuals with various wishes and concerns listed for the reader to circle which option he or she desired for himself or herself. The patient had circled the aforementioned option. The terms terminal and imminent became hot items for debate between the physician, who felt that it was too early to withdraw treatment based on her prior written wishes, and her family, who expressed their belief that the patient did not want to be on a ventilator at this time.
In the second case, several issues arose. The patient had the ability to give informed consent and to express her own wishes. In this case, directives given in a document should not take precedence over speaking to the patient, no matter how challenging it may be to find out his or her current wishes. No one thought initially to ask this patient what she wanted in terms of treatment modalities even though she had full capacity to make her own decisions; they chose instead to follow the available advance directive because they thought she had dementia. Only when the family request was different from what the healthcare team had planned did further analysis of the situation occur. Furthermore, while an advance directive was available for review, the patient had completed it approximately two decades earlier. Did the content included still represent her wishes? In addition, she was wrongly labeled as not having the capacity to make an informed decision because of her difficulty communicating due to an expressive aphasia. She was, in fact, able to express her wishes through the use of hand gestures and proved to all her ability to comprehend what was being told to her and to consistently let her wishes be known. Her wishes in this case were at odds with those of her family members and, given the fact that she did not have a terminal illness or imminent death, did not meet the criteria listed for withholding the feeding tube that was being urged by her family. The patient was, however, able to refuse it on her own since she had the capacity to make an informed decision regardless of what her family or her advance directive stated.
An advance directive delineates treatment preferences and may designate a surrogate decision-maker for the time when the individual is unable to make his or her own medical decisions. It should not be used if someone judged to have capacity is still able to express his or her desires about specific treatment options. Furthermore, the case 2 patient had named the “attorney at large,” not her family members, to be her surrogate if she was unable to make a decision on her own. The healthcare team not only initially failed to recognize that our patient had the capacity to make her own decisions, but also chose to discuss care options with her family rather than seek guidance from the “attorney at large,” if their judgment that she lacked capacity was accurate.
Conclusion
Our cases illustrate just how important it is that physicians discuss advance directives with their patients while they still have decision-making capacity. Specific details and wishes need to be clarified during such discussions. Additionally, surrogates and family members need to be made aware of patients’ wishes. Using uniform terminology and definitions when creating a living will can help remove any potential for ambiguity and variable interpretation of what patients’ wishes are. Patients need to understand the meanings of various terms before agreeing to what is being stated. Reimbursing physicians for their time to address end-of-life issues, including advance directive discussions, has recently been proposed without success. For now, a discussion regarding a patient’s advance directive is best included as part of a preventive care visit recognizing that, at least for the older patient, it will likely not receive the time it deserves due to many other competing demands on the physician’s time. Honoring patient wishes, respecting choices, and having advance directives that remove uncertainty and give clear instructions to healthcare providers are not only important to patients and their families, but also to our entire healthcare system. It can reduce patients’ suffering, alleviate caregiver burden, and reduce the burden on the healthcare system by helping to provide cost-effective care.
References
1. Wilkinson A, Wenger N, Shugarman LR; US Department of Health and Human Services. Literature review on advance directives of health and human services. Published June 2007. http://aspe.hhs.gov/daltcp/reports/2007/advdirlr.htm#note155. Accessed January 22, 2013.
2. Nabili ST. Advance medical directives (living will, power of attorney, and health-care proxy). www.medicinenet.com/advance_medical_directives/article.htm. Accessed January 22, 2013.
3. South Dakota Office of the Attorney General. Durable Power of Attorney. http://atg.sd.gov/Seniors/EstatePlanning/PowerofAttorney.aspx. Accessed January 22, 2013.
4. American Cancer Society. Advance directives. www.cancer.org/treatment/findingandpayingfortreatment/understandingfinancialandlegalmatters/advancedirectives/advance-directives-types-of-advance-health-care-directives. Accessed January 22, 2013.
5. The Library of Congress. Patient Self Determination Act (PSDA), Omnibus Reconciliation Act of 1990. http://thomas.loc.gov/cgi-bin/query/z?c101:H.R.4449.IH. Accessed January 26, 2013.
6. Hecht MB. Advance medical directives (living will, power of attorney, and health care proxy). www.medicinenet.com/script/main/art.asp?articlekey=7814. Accessed January 22, 2012.
7. Presidential Commission for the Study of Bioethical Issues. History of bioethics commissions. http://bioethics.gov/cms/history. Accessed January 22, 2013.
8. Cornell University Law School. Cruzan v. Director, Missouri Department of Health, (88-1503), 497 U.S. 261 (1990). www.law.cornell.edu/supct/html/88-1503.ZS.html. Accessed January 22, 2013.
9. Cornell University Law School. 10 USC § 1044c - Advance medical directives of members and dependents: requirement for recognition by States. Accessed January 22, 2013.
10. American College of Physicians. ACP Ethics Manual Sixth Edition. www.acponline.org/running_practice/ethics/manual/manual6th.htm#decisions-eol. Accessed January 22, 2013.
11. Competency to make legal decisions. www.stanford.edu/group/psylawseminar/Competency.htm. Accessed January 23, 2013.
12. Searight HR, Gafford J. Cultural diversity at the end of life: issues and guidelines for family physicians. Am Fam Physician. 2005;71(3):515-522.
13. Blackhall LJ, Frank G, Murphy ST, Michel V, Palmer JM, Azen SP. Ethnicity and attitudes towards life sustaining technology. Soc Sci Med. 1999;48(12):1779-1789.
14. Giger JN, Davidhizar RE, Fordham P. Multi-cultural and multi-ethnic considerations and advance d directives: developing cultural competency. J Cult Divers. 2006;13(1):3-9.
15. Hanson LC, Rodgman E. The use of living wills at the end of life. A national study. Arch Intern Med. 1996;156(9):1018-1022.
16. Duffield P, Pozamsky JE. The completion of advance directives in primary care. J Fam Pract. 1996;42:378-384.
17. Wissow LS, Belote A, Kramer W, et al. Promoting advance directive among elderly primary care patients. J Gen Intern Med. 2004;19(9):944-951.
Disclosures:
The authors report no relevant financial relationships.
Address correspondence to:
Steven R. Gambert, MD
University of Maryland Medical Center
N3E09, 22 S. Greene Street
Baltimore, MD 21201
sgambert@medicine.umaryland.edu


