Peer Reviewed
What Is This Painful Thigh Mass in an Older Woman?
AUTHORS:
Tobe Momah, MD, MSc1 • Ewaenosa Ukponmwan, MD2
AFFILIATIONS:
1Department of Family Medicine, University of Mississippi Medical Center, Jackson, Mississippi
2College of Medicine, University of Benin, Benin City, Nigeria
CITATION:
Momah T, Ukponmwan E. Atypical liposarcoma tumor of the left thigh. Consultant. 2021;61(7):e14-e15. doi:10.25270/con.2021.03.00013
Received October 8, 2020. Accepted January 18, 2021. Published online March 16, 2021.
DISCLOSURES:
The authors report no relevant financial relationships.
CORRESPONDENCE:
Tobe Momah, MD, MSc, Department of Family Medicine, University of Mississippi Medical Center, 764 Lakeland Drive, Jackson, MI 39216 (tmomah@umc.edu)
An 83-year-old woman presented to our clinic with abnormal swelling in the left thigh (Figure 1). The patient’s swelling had been present for more than 10 years and was progressively increasing in size. She had a medical history of dementia, hypertension, anemia, and type 2 diabetes and denied history of trauma to the left thigh or falls.

Figure 1. The patient had presented with progressive swelling in the left thigh.
She had undergone magnetic resonance imaging (MRI) of the left thigh without contrast, results of which showed a 39-cm fat-containing mass (Figure 2). The patient denied any pain in the left thigh but reported progressive and increased swelling at the site.
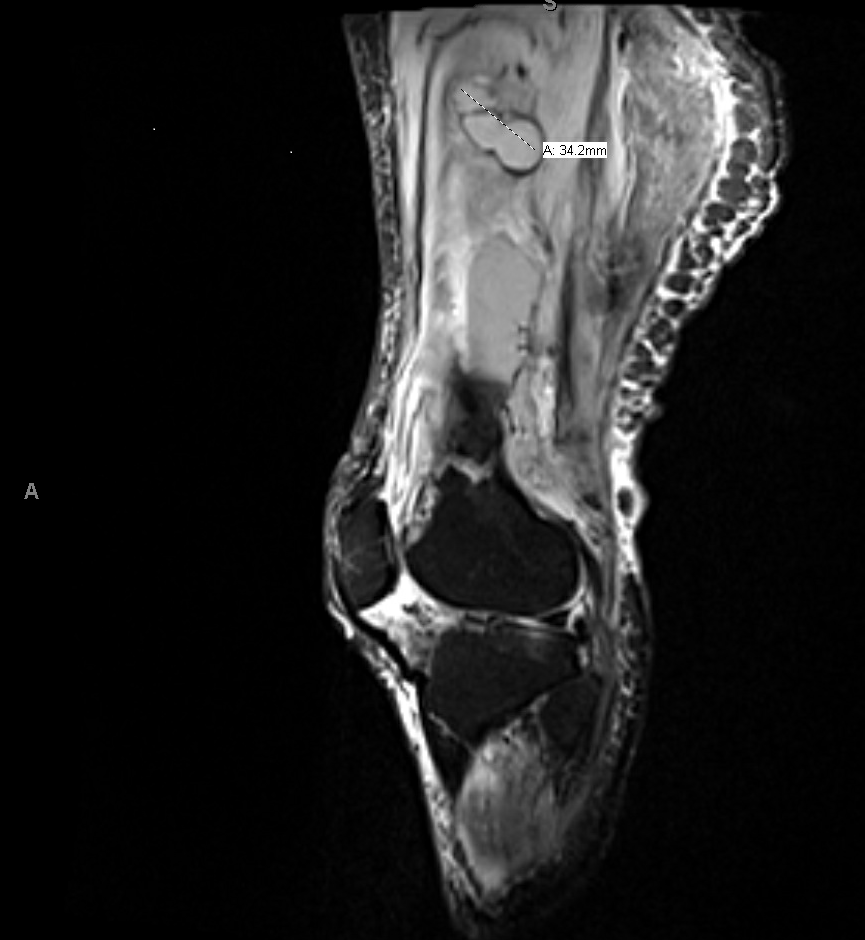
Figure 2. MRI scan showed a 39-cm fat-containing mass.
Answer and discussion on next page.
Correct answer: D. Liposarcoma
The MRI scan showed a fat-containing mass compatible with a liposarcoma.
The patient subsequently underwent an ultrasound-guided biopsy of the mass, results of which demonstrated an atypical lipomatous tumor, or well-differentiated liposarcoma, with MDM2-positive cytogenecity. Three months later, she underwent wide resection of mass. Histopathology results showed a tumor measuring 43.8 × 33.2 × 4.8 cm, with extension into the peripheral resection margins at multiple foci but with no lymphovascular invasion. The American Joint Committee on Cancer pathological staging of this lesion was a pT4 pNx well-differentiated low-grade liposarcoma. This staging is due to the tumor extending to the peripheral resection margins at multiple foci, with nil mitosis and no lymphovascular invasion identified.
The patient was discharged to a rehabilitation facility but was readmitted to the hospital one month later with postoperative complications, including a 21-cm abscess surrounding the mid-distal femur, a 4-cm abscess in the distal semimembranosus muscle, and deep venous thrombus in the left mid-femoral vein.
Wound cultures were taken, results of which were positive for methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa. Results of a urinalysis were positive for Escherichia coli. The patient was started on 28 days of intravenous antibiotics (including vancomycin and ciprofloxacin), an anticoagulant (rivaroxaban), and an anti-Alzheimer medication (donepezil).
Discussion. Liposarcoma tumors are rare malignant tumors that arise from adipose tissue, with an annual incidence of 2.5 cases per million population.1 They are the most common soft tissue tumor and account for 20% of all sarcoma cases in adults.2 Liposarcomas are classified into 4 clinical subtypes: well-differentiated, dedifferentiated, myxoid, and pleomorphic. Well-differentiated liposarcoma is the most common subtype. They are indolent in behavior, have a high risk of local recurrence, and are insensitive to radiotherapy and chemotherapy.3 They are usually not metastatic unless they have a dedifferentiated component, and patient outcomes are usually good when the mass is completely excised.3
The 5-year disease-specific survival in patients with pure well-differentiated liposarcoma is 93%. The location of well-differentiated liposarcoma is an important prognostic factor. Retroperitoneal tumors are more prone to recurrence than tumors of the extremities.2 On imaging, a well-differentiated liposarcoma appears as a lipomatous mass with similar signal intensity as normal fat.2
Our patient had a well-differentiated liposarcoma, otherwise called atypical lipoma. Since the margins were positive, she had a risk of local recurrence. In the patient population aged between 60 to 80 years, well-differentiated liposarcoma is more common than dedifferentiated liposarcoma.5 Well-differentiated liposarcoma is also more common in the lower extremities, as seen in our patient.5 Surgery is the mainstay of treatment for well-differentiated liposarcoma, and our patient had a wide resection of the tumor. Radiation therapy is not recommended after resection of well-differentiated liposarcoma in the extremities, because death from the disease is rare even in cases of recurrence.4
The tumor reduced the patient’s ability to participate in independent activities of daily living and limited her ability to ambulate or bend her knee, which—in addition to her age—increased her morbidity and mortality risk. Because of the patient’s Alzheimer dementia, she could not express her pain qualitatively. The tumor had been present for more than 10 years, and its increased size and timeline predisposed her to an increased risk of dedifferentiation, which would be high risk for not only continued growth but metastatic development. The high risk of local recurrence, dedifferentiated liposarcoma rising out of the well-differentiated liposarcoma tumor, and metastasis necessitated her surgery.
Patient outcome. Our patient was referred to a skilled nursing home and was eventually moved to home hospice after 2 further hospital admissions for worsening left thigh pain and decreased mental status. Since the surgery, she had had a debilitated state of health with impaired ambulation and an inability to perform activities of daily living. Her placement in hospice was in tandem with her family’s wishes. The patient died 6 months after the wide excision surgery was performed to treat the well-differentiated liposarcoma.
Our patient’s post-operative complications were greater than estimated. This case highlights the poor prognosis in patients with dementia who present with poor ambulation and impaired coordination (especially in terms of postoperative physical therapy) and the need to galvanize social, medical, physical, and psychological factors in determining a patient’s suitability for surgery.
References
- Al-Zaid T, Frieling G, Rosenthal S. Dermal pleomorphic liposarcoma resembling pleomorphic fibroma: report of a case and review of the literature. J Cutan Pathol. 2013;40(8):734-739. https://doi.org/10.1111/cup.12164
- Bill KLJ, Casadei L, Prudner BC, Iwenofu H, Strohecker AM, Pollock RE. Liposarcoma: molecular targets and therapeutic implications. Cell Mol Life Sci. 2016;73(19):3711-3718. https://doi.org/10.1007/s00018-016-2266-2
- Lee ATJ, Thway K, Huang PH, Jones RL. Clinical and molecular spectrum of liposarcoma. J Clin Oncol. 2018;36(2):151-159. https://doi.org/10.1200/jco.2017.74.9598
- Crago AM, Dickson MA. Liposarcoma: multimodality management and future targeted therapies. Surg Oncol Clin N Am. 2016;25(4):761-773. https://www.surgonc.theclinics.com/article/S1055-3207(16)30020-5/fulltext
- Thway K. Well-differentiated liposarcoma and dedifferentiated liposarcoma: an updated review. Semin Diagn Pathol. 2019:36(2):112-121. https://doi.org/10.1053/j.semdp.2019.02.006


