Comparing Prior Radiographs Aids in the Diagnosis of Bronchiectasis
Authors:
Sudip Sheth, MD, MPH; Adaobi Kanu, MD; and Curtis Turner, MD
Citation:
Sheth S, Kanu A, Turner C. Comparing prior radiographs aids in the diagnosis of bronchiectasis. Consult Pediatricians. 2015;14(11):504-506.
A 2-year-old girl presented with a 1-day history of high-grade fever, cough, and rhinorrhea. She was lethargic and had decreased oral intake. She had no sick contacts or choking episodes.
On admission, her temperature was 40°C, her heart rate was 148 beats/min, and her respiratory rate was 45 breaths/min with moderate respiratory distress. Physical examination revealed bilateral expiratory wheezes with decreased air entry in the right upper chest.
The girl had been hospitalized 3 times in the past for presumptive aspiration pneumonia, beginning at 1 month of age. At 15 months of age, results of a modified barium swallow study demonstrated severe aspiration, and so she underwent gastrostomy feeding tube placement.
Her current medications included albuterol, 2.5 mg every 4 hours as needed via nebulizer, and budesonide, 0.5 µg twice a day.
Treatment was started with parenteral clindamycin for presumptive aspiration pneumonia of the right upper lobe. All of her previous radiographs were reviewed (Figures 1-3), and a computed tomography scan of the chest was performed (Figure 4), the latter of which revealed bronchiectasis. Results of a quantitative sweat test were negative for cystic fibrosis, and results of immune function testing were normal.

Figure 1: Chest radiograph of the patient at 1 month of age.
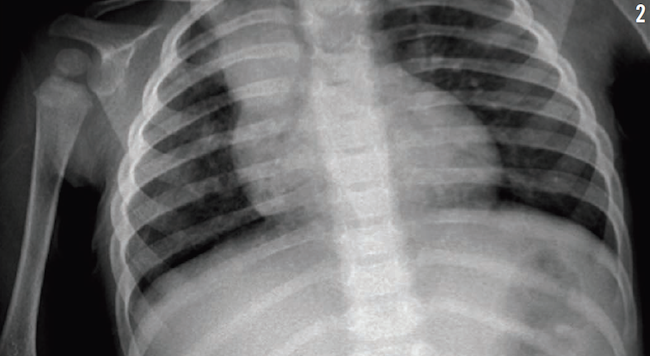
Figure 2: Chest radiograph of the patient at 15 months of age.

Figure 3: Chest radiograph of the patient at 33 months of age.
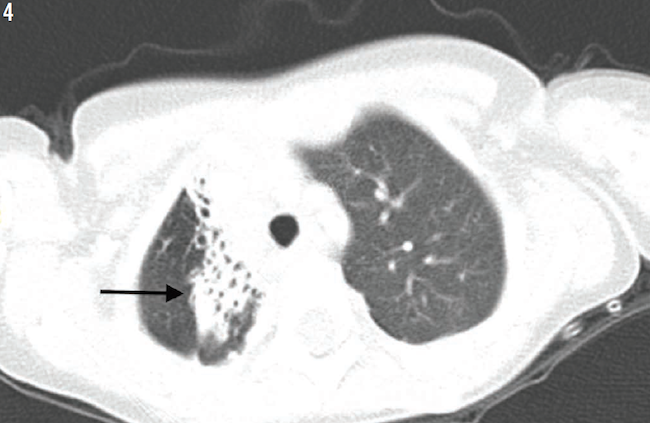
Figure 4: High-resolution computed tomography scan of the patient at 33 months of age demonstrated infiltrate with an area of bronchiectasis (arrow).
Bronchiectasis is an injury to the bronchi, resulting in dilatation. It can be categorized according to the pathologic or radiographic appearance of airways.1 Chronic aspiration pneumonia is a frequent cause of bronchiectasis.2 High-resolution computed tomography (HRCT) is the most sensitive imaging method for the diagnosis of bronchiectasis.3 The initial management in aspiration-related bronchiectasis is to diagnose and treat the cause of aspiration.4
Some authors recommend that HRCT should be considered earlier when there is a clinical suspicion of aspiration, especially on chest radiographs.5 Comparing the previous chest radiographs with current ones can aid in the early identification of bronchiectasis and alter the management and prognosis of the condition. Omitting the comparison of prior radiographs may delay the diagnosis of bronchiectasis.
Sudip Sheth, MD, MPH, is a resident pediatrician in the Department of Pediatrics at Texas Tech University Health Sciences Center at Amarillo.
Adaobi Kanu, MD, is an associate professor of pediatrics in the Division of Pulmonology, Department of Pediatrics, at Texas Tech University Health Sciences Center at Lubbock.
Curtis Turner, MD, is a professor of pediatrics in the Division of Hematology and Oncology, Department of Pediatrics, at Texas Tech University Health Sciences Center at Amarillo.
References:
- Reid LM. Reduction in bronchial subdivision in bronchiectasis. Thorax. 1950;5(3):233-247.
- Piccione JC, McPhail GL, Fenchel MC, Brody AS, Boesch RP. Bronchiectasis in chronic pulmonary aspiration: risk factors and clinical implications. Pediatr Pulmonol. 2012;47(5):447-452.
- Smith IE, Flower CDR. Review article: imaging in bronchiectasis. Br J Radiol. 1996;69(823):589-593.
- Boesch RP, Daines C, Willging JP, et al. Advances in the diagnosis and management of chronic pulmonary aspiration in children. Eur Respir J. 2006;28(4):847-861.
- Barker AF. Bronchiectasis. N Engl J Med. 2002;346(18):1383-1393.


